Lindy Stotsky, known to many of you by her Twitter name @EMRAnswers, gave a compelling and compassionate account at HIMSS15 of how the lack of access to patient records — by clinicians, patients, and especially family members/caregivers— failed her mother during her stay in a long-term care facility. Her story, appended below, resonated with the audience and led several other people to describe how experiences trying to navigate the healthcare system without full access to information from health records spurred them to become involved in health IT.
I followed Linda with a story of how my mother became interested in examining the data in her health record only after I prodded her primary care practice to provide access, once I realized that they had implemented a patient portal.
It was notable that most of the personal stories from the audience that followed Linda & my brief talks at the #IHeartHIT session related to caring for our Moms. I want to thank Linda for sharing her story here on the Health Content Advisors site.
I Was My Mother’s “Scrap of Paper”
I’ve worked in healthcare over 25 years: In administration through hospital credentialing and procurement, as a practice administrator shuffling through paper charts, missing codes, and reimbursement in an era of managed care. It was during this time that my Mother became ill with CLL (Chronic Lymphocytic Leukemia), and COPD (Chronic Obstructive Pulmonary Disorder). My Mother was a staunch believer in Health CARE. She grew up believing that physicians were healers- and that nursing facilities took care of the elderly. Her decision to reside in such a facility began our descent into a world I could not have imagined. 
I looked, as most caregivers do, at the inside of the building, the floors, the paint and the aesthetics. We are preoccupied, vulnerable and first impressions are everything. I judged the worthiness of the facility by its locale, the staff and our welcome. I took for granted that “Nurses” were RN’s, having an MD as Chief of Staff meant he was there every day, and daily living meant more than struggling to survive. I didn’t know about physician track records, medical malpractice and negligence. All blue skies and daisies, until my Mom became a resident. That started our fragile dance between long-term care (LTC), emergency departments (ED), hospital, provider, back to LTC.
Thus began my advocacy. Not just for MY Mom. I was vigilant about everyone’s Mom— policing halls, looking into rooms, and answering cries for help. I watched my Mother change from a vibrant, confident superhero to a terrified, confused and helpless patient. I took her to providers who placed her on medication, only to bring her back to a facility where medications were routinely discontinued because of cost.
I was “on call” 24/7. My Mom became my mission. My 3 year old knew where all the toys were kept in the ED, as we were frequent fliers. “AMA” meant no ambulance was ever called. I loaded her, her wheelchair, her O2 tank, and my son into the car, and as I was running out, I grabbed a piece of notebook paper with her medications scribbled on it. This was her medical record. And I was the keeper of the key information.
My Mother passed away after three years of suffering, much of which was preventable. Not only was there a lack of communication, a culture of caring had been replaced by one of cost. Human lives took a back seat to ROI. Instead of treating aging elders with the respect and dignity they deserved after years of giving, nursing homes were nothing more than “death beds” waiting to empty. I was so engrossed in the day to day challenges, that I didn’t have time to stop and think about the larger picture of what was wrong.
15 years later I am sorry to say that things have not changed much. My daughter recently had Thyroid Cancer. She was eager to use the patient portal to coordinate her labs, multiple tests, from all providers. It was not that easy. Information gaps were everywhere; care coordination was still back in the year 2000. We need patient access. But it’s more than that. We need actionable information. It’s been nearly five years since the enactment of the ACA and little has been done to promote shared decision making. The recent proposed rule change in the Meaningful Use Stage 2 measure related to patient access and downloading of their information[1] will reduce the threshold for Measure 2 from 5% to “at least 1 patient” for eligible providers (EP). This change HALTS progress. WE CAN DO BETTER. My daughter is working hard to be a partner in her care, yet she has a toddler, and she’s tired, and sometimes it’s easier to give up rather than continue asking.
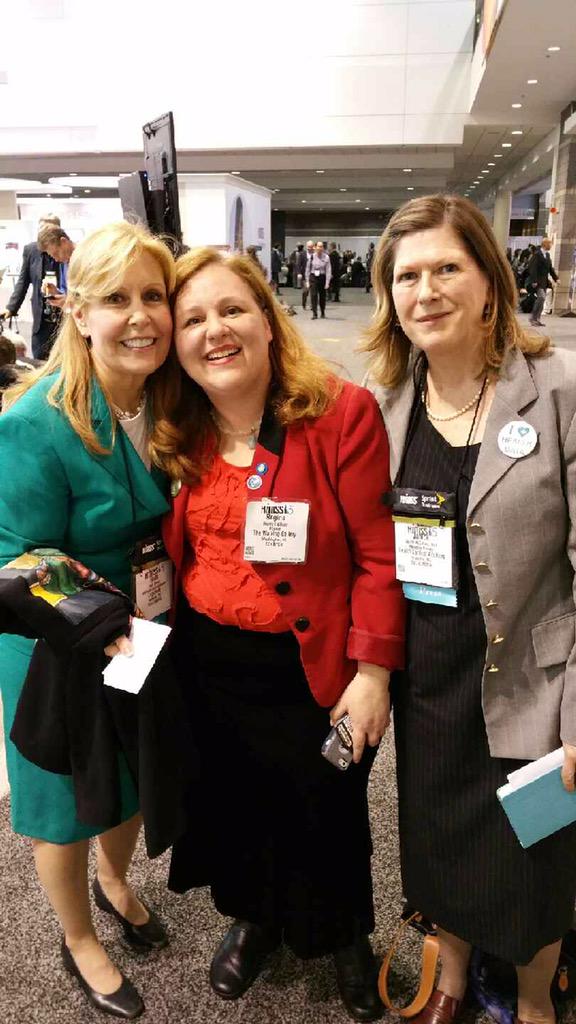 Linda, Regina Holliday and me at HIMSS15
Linda, Regina Holliday and me at HIMSS15
Please help us win this. Stand up and ask —-demand electronic access to your patient record. We should not have to carry around a tattered scrap of paper with medical information on it. Join members of The Walking Gallery[2] of Healthcare as we tell HHS, CMS, Politicians and Advocates that PATIENT LIVES MATTER.
My name is Linda Stotsky, and I share my story as a patient, a caregiver, a Mom, a daughter and a Health IT Product Manager. I am currently the Director of Business Development at LogicNets.
I can be reached at Linda.Stotsky@gmail.com or on Twitter via @EMRAnswers
[1] http://e-patients.net/archives/2015/05/add-your-voice-meaningful-use-regulations-musnt-leave-patient-engagement-in-the-dust.html
[2] For information on TheWalking Gallery, see http://reginaholliday.blogspot.com/2011/04/walking-gallery.html.